Introduction to Pelvic Organ Prolapse
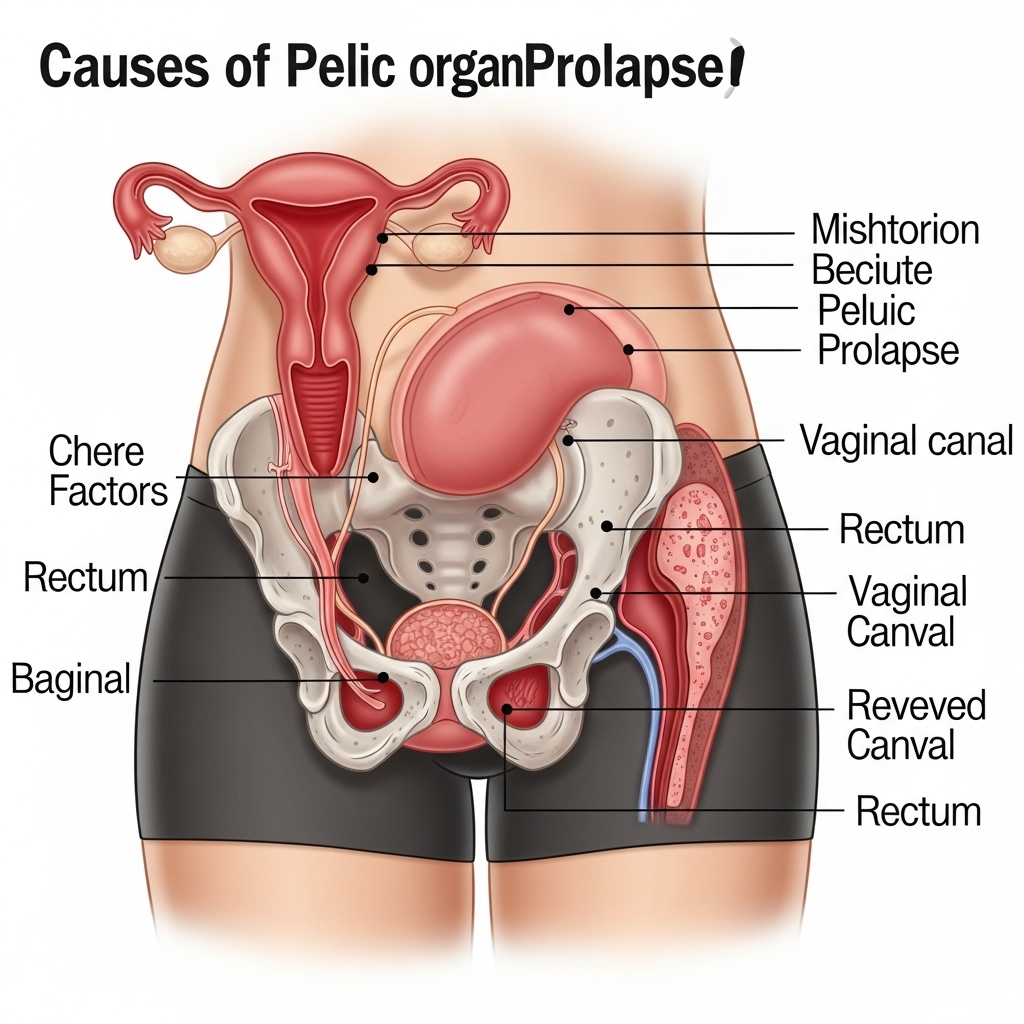
Pelvic organ prolapse (POP) is a condition that affects many postmenopausal women, causing significant discomfort, pain, and disruption to daily life. It occurs when the muscles and tissues that support the pelvic organs, such as the bladder, uterus, and bowel, weaken and allow these organs to bulge or prolapse into the vagina. This can lead to a range of symptoms, including pelvic pressure, urinary incontinence, and difficulty with bowel movements. In this article, we will explore the causes of pelvic organ prolapse in postmenopausal women, and discuss the factors that contribute to its development.
Menopause and Hormonal Changes
Menopause is a significant factor in the development of pelvic organ prolapse. During menopause, the levels of estrogen in the body decrease, leading to a range of changes that can affect the pelvic floor. Estrogen helps to maintain the strength and elasticity of the muscles and tissues that support the pelvic organs. When estrogen levels decline, these tissues can become weaker and more prone to prolapse. For example, a study published in the Journal of Women's Health found that women who experienced a significant decline in estrogen levels during menopause were more likely to develop pelvic organ prolapse.
Age-Related Changes
As women age, they undergo a range of physical changes that can contribute to the development of pelvic organ prolapse. The muscles and tissues that support the pelvic organs can become weaker and less elastic, making them more prone to prolapse. Additionally, the pelvic floor can become less able to withstand the forces of gravity, coughing, and straining, which can put additional pressure on the pelvic organs. For instance, a woman who has had multiple pregnancies and vaginal deliveries may experience a weakening of the pelvic floor muscles, making her more susceptible to prolapse as she ages.
Obesity and Increased Intra-Abdominal Pressure
Obesity is another factor that can contribute to the development of pelvic organ prolapse. Excess weight can put additional pressure on the pelvic floor, causing the muscles and tissues to weaken and become more prone to prolapse. This is because the increased intra-abdominal pressure can cause the pelvic organs to bulge into the vagina, leading to prolapse. For example, a study published in the International Urogynecology Journal found that obese women were more likely to experience pelvic organ prolapse than women of a healthy weight.
Genetic Predisposition and Family History
Genetic factors can also play a role in the development of pelvic organ prolapse. Women who have a family history of prolapse are more likely to experience it themselves. This may be due to inherited traits such as weaker connective tissue or a predisposition to pelvic floor weakness. Additionally, certain genetic conditions, such as Ehlers-Danlos syndrome, can increase the risk of pelvic organ prolapse. For instance, a woman whose mother or sister has experienced prolapse may be more likely to develop it herself, even if she has not had any other risk factors.
Other Medical Conditions and Factors
Certain medical conditions, such as chronic coughing or constipation, can also contribute to the development of pelvic organ prolapse. These conditions can put additional pressure on the pelvic floor, causing the muscles and tissues to weaken and become more prone to prolapse. Additionally, women who have had a hysterectomy or other pelvic surgery may be at increased risk of developing prolapse. For example, a woman who has chronic obstructive pulmonary disease (COPD) and experiences frequent coughing may be more likely to develop prolapse due to the increased pressure on her pelvic floor.
Treatment and Prevention
While pelvic organ prolapse can be a challenging condition to manage, there are a range of treatment options available. These can include pelvic floor exercises, such as Kegel exercises, which can help to strengthen the muscles that support the pelvic organs. Additionally, women may be advised to make lifestyle changes, such as losing weight or avoiding heavy lifting, to reduce the pressure on their pelvic floor. In some cases, surgery may be necessary to repair the prolapse and restore the normal position of the pelvic organs. For instance, a woman who has experienced a significant prolapse may undergo a surgical procedure to repair the damaged tissues and restore the normal anatomy of her pelvic floor.
Conclusion
In conclusion, pelvic organ prolapse is a complex condition that can be caused by a range of factors, including menopause, age-related changes, obesity, genetic predisposition, and certain medical conditions. Understanding these factors can help women to take steps to prevent prolapse, such as maintaining a healthy weight, practicing pelvic floor exercises, and avoiding heavy lifting. Additionally, women who are experiencing symptoms of prolapse should seek medical attention, as early treatment can help to prevent further complications and improve quality of life. By working together with their healthcare providers, women can take control of their pelvic health and reduce their risk of developing this debilitating condition.
