Introduction to Sleep Position and Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a common sleep disorder characterized by repeated episodes of partial or complete upper airway obstruction during sleep, resulting in disrupted sleep and decreased oxygen levels in the blood. The severity of OSA symptoms can vary significantly among individuals, and several factors contribute to this variability, including sleep position. This article will explore the relationship between sleep position and the severity of OSA symptoms, discussing the mechanisms, research findings, and implications for treatment and management.
Understanding Obstructive Sleep Apnea
OSA occurs when the muscles in the throat relax and collapse, blocking the airway and preventing normal breathing. This can happen multiple times throughout the night, leading to fragmented sleep and daytime fatigue. The severity of OSA is typically measured by the apnea-hypopnea index (AHI), which represents the number of apneic and hypopneic events per hour of sleep. A higher AHI indicates more severe OSA. Factors such as obesity, age, and craniofacial anatomy can influence the severity of OSA, but sleep position also plays a crucial role.
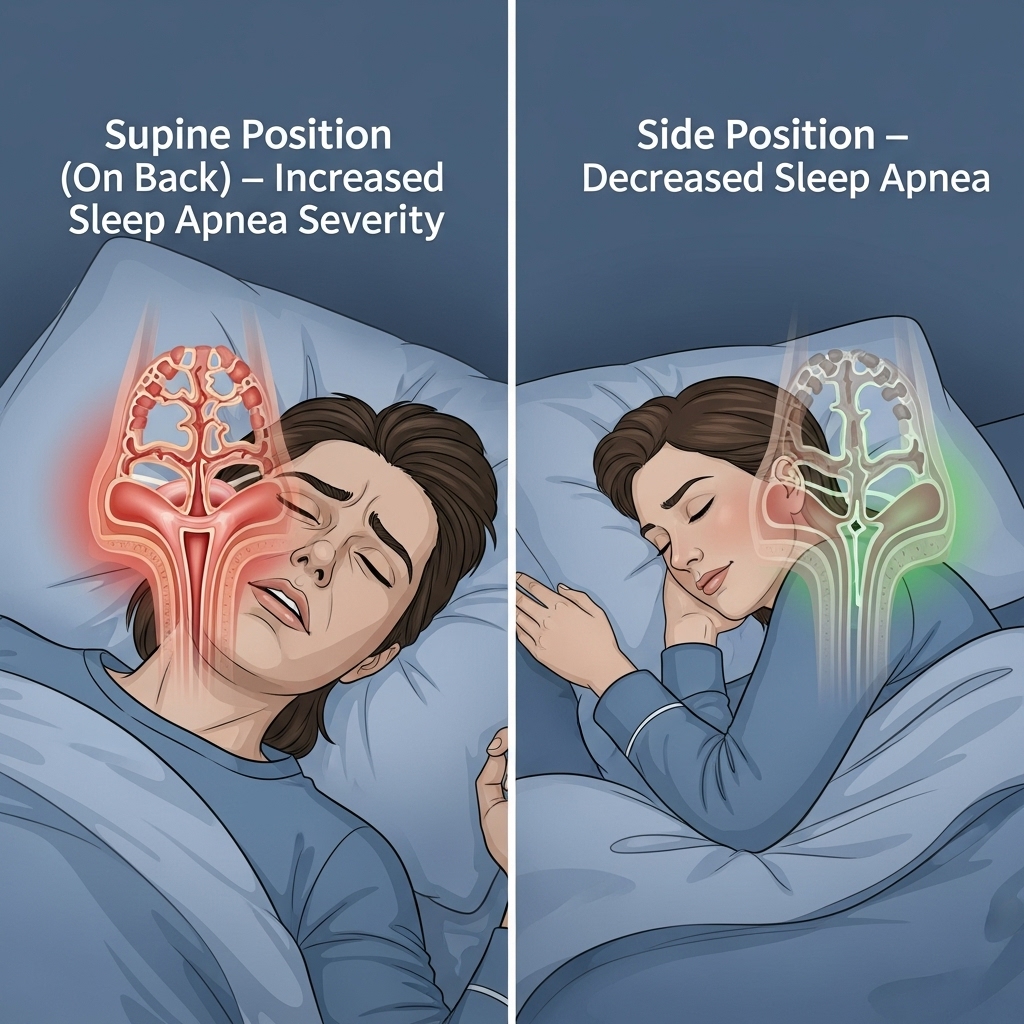
Sleep Position and Upper Airway Patency
The position in which a person sleeps can significantly affect the patency of the upper airway. When sleeping on the back (supine position), gravity can cause the jaw and soft tissues of the throat to fall back and obstruct the airway, exacerbating OSA symptoms. In contrast, sleeping on the side (lateral position) can help keep the airway open by preventing the jaw and soft tissues from falling back. This is because the lateral position allows the mandible to move forward, increasing the diameter of the upper airway and reducing the likelihood of obstruction.
Research Findings on Sleep Position and OSA Severity
Several studies have investigated the relationship between sleep position and OSA severity. A systematic review of 22 studies found that sleeping in the supine position was associated with a higher AHI and more severe OSA symptoms compared to sleeping in the lateral position. Another study using polysomnography (PSG) to monitor sleep and breathing patterns found that OSA patients who slept on their backs had a significantly higher AHI and longer apneic events than those who slept on their sides. These findings suggest that sleep position can have a profound impact on the severity of OSA symptoms.
Examples of Positional Therapy for OSA
Positional therapy, which involves training patients to sleep in a non-supine position, has been shown to be effective in reducing OSA severity. For example, a study using a positional therapy device that prevented patients from sleeping on their backs found a significant reduction in AHI and improvement in sleep quality. Another example is the use of tennis balls sewn into the back of a shirt to discourage back sleeping. These interventions can be simple and cost-effective ways to manage OSA symptoms, especially for patients with mild to moderate disease.
Implications for Treatment and Management
The relationship between sleep position and OSA severity has important implications for treatment and management. For patients with positional OSA, which is defined as an AHI that is at least twice as high in the supine position as in the lateral position, positional therapy may be a viable treatment option. Additionally, sleep position should be considered when diagnosing and treating OSA, as patients who sleep on their backs may require more aggressive treatment. Furthermore, educating patients about the importance of sleep position and providing them with strategies to maintain a non-supine position during sleep can be a valuable adjunct to other treatments, such as continuous positive airway pressure (CPAP) therapy.
Conclusion
In conclusion, the relationship between sleep position and the severity of OSA symptoms is complex and multifaceted. Sleeping on the back can exacerbate OSA symptoms by increasing upper airway obstruction, while sleeping on the side can help keep the airway open. Research findings and examples of positional therapy demonstrate the importance of considering sleep position in the diagnosis, treatment, and management of OSA. By understanding the impact of sleep position on OSA severity and incorporating positional therapy into treatment plans, healthcare providers can help improve sleep quality and reduce the risk of complications associated with OSA.
